RBI Impact
Care That Delivers Measurable Success
RBI delivers more than expertise, we deliver results. With measurable improvements in stroke response, treatment speed, and patient recovery, we help hospitals provide better care that leads to better patient outcomes.
Better Care Leads to Real Results
RBI is redefining stroke and neurological care by equipping hospitals with expert training and advanced protocols while ensuring every patient receives the highest standard of care. By improving stroke recognition, reducing treatment delays, and expanding neurology services, we help hospitals deliver faster, safer, and more effective care. The result? More lives saved, better recoveries, and stronger communities.
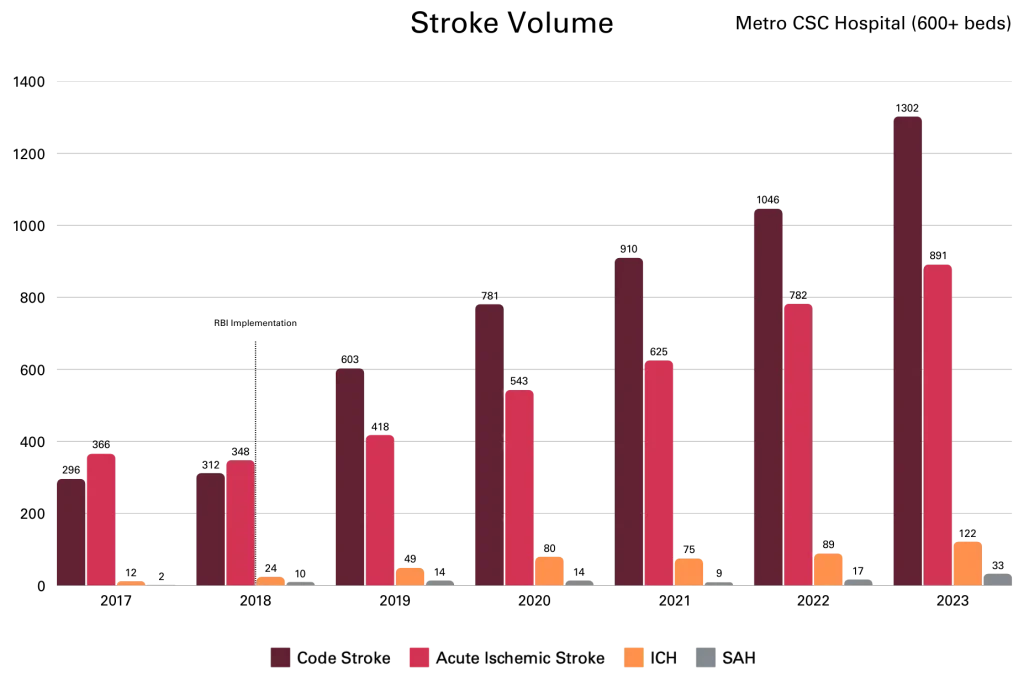
Increased Stroke Volume: Becoming a Magnet for Stroke Care
Before RBI, hospitals under-called code stroke, leading to missed, misdiagnosed, or delayed treatments. In 2017, this hospital called only 296 code strokes despite 366 actual ischemic strokes. Underutilization leads to delayed interventions and worse outcomes.
With RBI’s training, stroke recognition improved, leading to more accurate code stroke activations, not just more calls, but more confirmed strokes (ischemic, ICH, and SAH). As care improved, the hospital became a preferred stroke center, attracting more cases from EMS and referring hospitals. It didn’t just get better at treating strokes, it became a trusted destination for stroke care.
Key Takeaways from the Data:
- More strokes caught and treated—Hospitals now activate stroke protocols earlier and more accurately.
- More ischemic strokes, ICH, and SAH cases were caught and treated, proving more accurate stroke recognition.
- Hospitals with strong stroke programs attract more patients—increased EMS arrivals and referrals sustained growth.
This data confirms what we see across all RBI partner hospitals: when you build a strong stroke program, stroke volume naturally increases. Hospitals don’t just improve—they become regional leaders in stroke care, ensuring more patients receive the treatment they need when seconds matter most.
Decreased Stroke Transfers: Keeping Patients Close to Home
Before RBI’s intervention, hospitals frequently transferred stroke patients to larger facilities, believing they lacked the capacity to treat them on-site. This led to delays in treatment, added strain on tertiary stroke centers, and increased stress for patients and families.
The graph illustrates a dramatic and sustained decline in stroke transfers following RBI’s intervention. Initially, transfer rates were high, but as hospitals became more confident and equipped to handle strokes locally, transfers decreased and then stabilized at a significantly lower rate.
Key Takeaways from the Data:
- Significant drop in transfers after RBI intervention—Hospitals retained and treated more stroke patients locally.
- Rapid decline, then stabilization—A sharp initial decrease shows the immediate impact of improved training and stroke protocols, followed by a steady, sustainable reduction.
- Hospitals became stroke-ready—Instead of immediately transferring patients, providers developed the expertise and confidence to assess, diagnose, and treat strokes on-site.
RBI’s impact is clear, hospitals don’t just recognize strokes better, they treat them better. By reducing transfers and strengthening local stroke care, more patients receive the right treatment at the right time, without having to leave their communities.
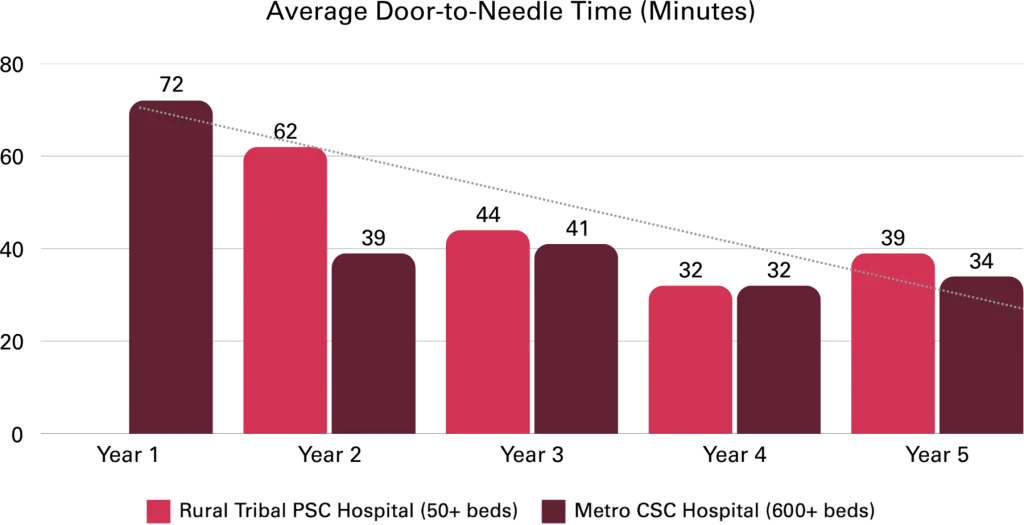
Provided Fast, Safe Treatment: Faster Action, Better Outcomes, Safer Care
Time is critical in stroke care. Before RBI’s intervention, hospitals often struggled with slow response times, delayed treatment, and higher complication rates. Many stroke teams took too long to activate, and door-to-needle times frequently exceeded the recommended treatment window.
RBI introduced standardized protocols, hands-on training, and streamlined activation processes, ensuring that stroke teams responded faster, treatment was administered sooner, and patient safety remained a top priority.
Key Takeaways from the Data:
- Faster Stroke Team Activation – Median door-to-stroke team time became three times faster than the national goal of under 15 minutes.
- Reduced Door-to-Needle Times – Treatment is now administered in under 30 minutes, ensuring more patients receive tPA within the critical window.
- Safer Stroke Treatment – RBI-trained hospitals maintain a 2.2% tPA hemorrhagic conversion rate, significantly lower than the 6% national average.
With RBI’s expertise, stroke teams don’t just work faster—they work smarter and safer. These improvements ensure that every second counts, every treatment is timely, and every patient has the best chance at recovery.
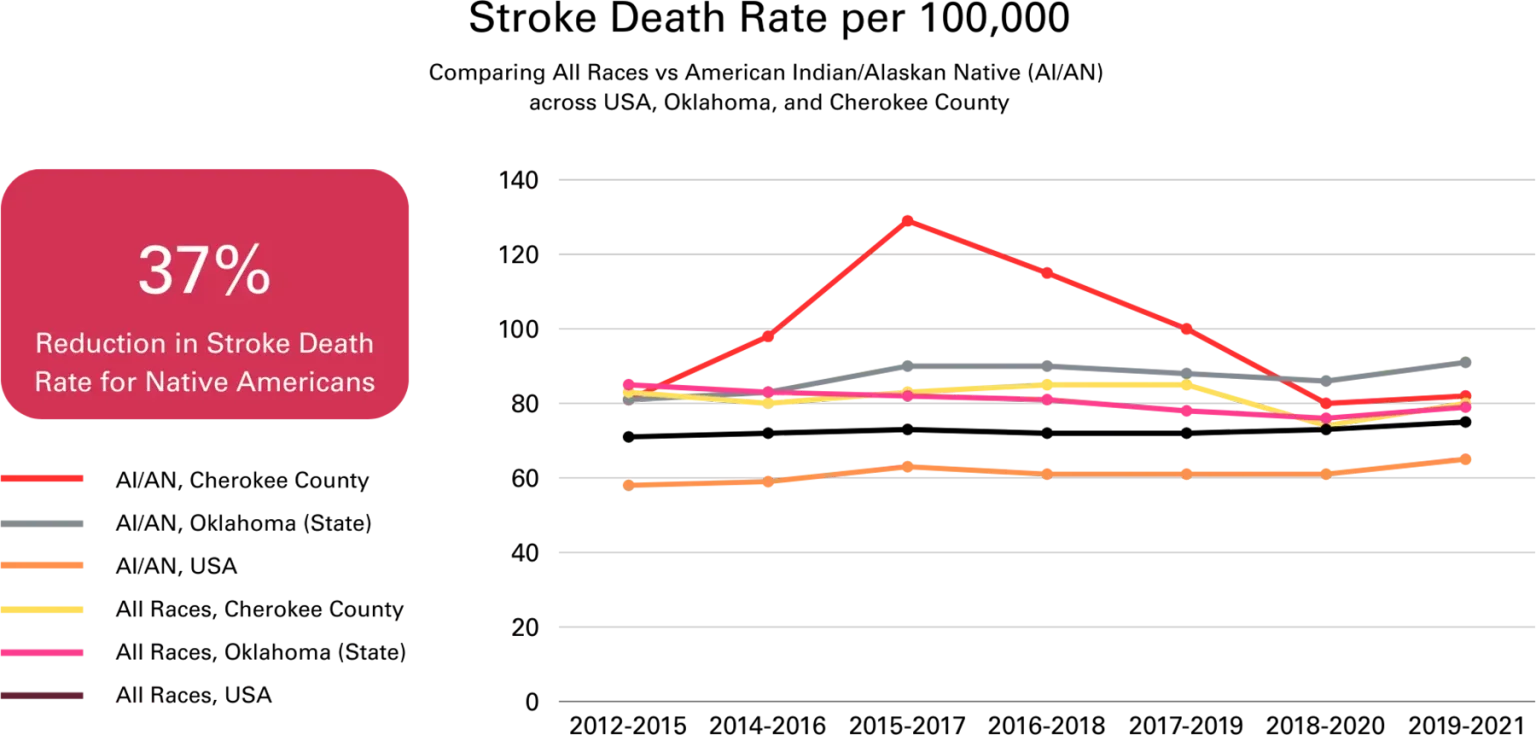
Achieved Extraordinary Patient Outcomes: Saving More Lives, Improving Recoveries
Stroke care isn’t just about survival, it’s about ensuring patients regain independence and quality of life. RBI’s approach has led to dramatic improvements in both survival rates and neurological recovery.
Key Takeaways from the Data:
- 37% reduction in stroke death rate for Native Americans—ensuring more patients survive and recover.
- 73% fewer neurological deficits (NIHSS score improvement) at discharge—meaning patients leave the hospital in far better condition.
- 52% of patients fully recovered—regaining normal neurological function.
- 84% of patients regained full independence—discharged with minimal to no long-term disability.
RBI’s impact is measurable, life-changing, and unmatched. By combining expert-led training, advanced stroke protocols, and a commitment to patient-centered care, we’re redefining what’s possible in stroke treatment and recovery.
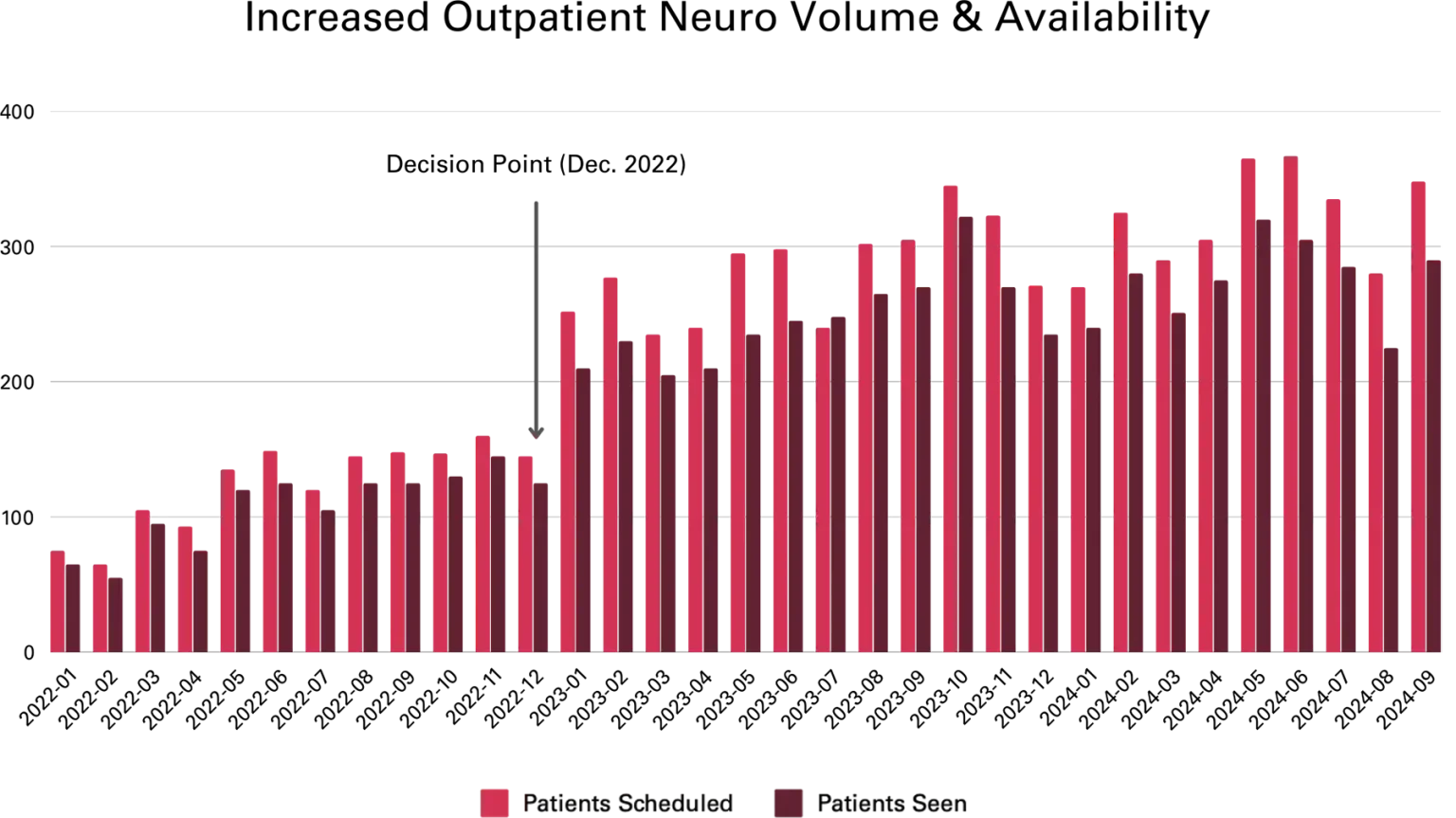
Robust Outpatient Neuro Clinic Capacity: Expanding Access, Preventing Stroke
The ability to provide timely, high-quality outpatient neurology care is critical to preventing both initial and recurrent strokes. RBI has helped hospitals significantly expand their outpatient neuro capacity, ensuring more patients receive specialized neurological care faster than ever before.
Key Takeaways from the Data:
- Increased patient volume while maintaining high-quality care
- Cleared a 900-patient backlog 18 months ahead of schedule
- Established fellowship-trained subspecialty clinics, including MS, headache, and movement disorder clinics
This growth directly impacts stroke prevention—patients who receive timely neurological care are less likely to experience secondary strokes. With more patients seen sooner and highly trained specialists available, RBI is breaking the cycle of recurrent stroke and improving long-term neurological health.
Increased Stroke Volume: Becoming a Magnet for Stroke Care
Before RBI, hospitals under-called code stroke, leading to missed, misdiagnosed, or delayed treatments. In 2017, this hospital called only 296 code strokes despite 366 actual ischemic strokes. Underutilization leads to delayed interventions and worse outcomes.
With RBI’s training, stroke recognition improved, leading to more accurate code stroke activations, not just more calls, but more confirmed strokes (ischemic, ICH, and SAH). As care improved, the hospital became a preferred stroke center, attracting more cases from EMS and referring hospitals. It didn’t just get better at treating strokes, it became a trusted destination for stroke care.
Key Takeaways from the Data:
- More strokes caught and treated—Hospitals now activate stroke protocols earlier and more accurately.
- More ischemic strokes, ICH, and SAH cases were caught and treated, proving more accurate stroke recognition.
- Hospitals with strong stroke programs attract more patients—increased EMS arrivals and referrals sustained growth.
This data confirms what we see across all RBI partner hospitals: when you build a strong stroke program, stroke volume naturally increases. Hospitals don’t just improve—they become regional leaders in stroke care, ensuring more patients receive the treatment they need when seconds matter most.
Decreased Stroke Transfers: Keeping Patients Close to Home
Before RBI’s intervention, hospitals frequently transferred stroke patients to larger facilities, believing they lacked the capacity to treat them on-site. This led to delays in treatment, added strain on tertiary stroke centers, and increased stress for patients and families.
The graph illustrates a dramatic and sustained decline in stroke transfers following RBI’s intervention. Initially, transfer rates were high, but as hospitals became more confident and equipped to handle strokes locally, transfers decreased and then stabilized at a significantly lower rate.
Key Takeaways from the Data:
- Significant drop in transfers after RBI intervention—Hospitals retained and treated more stroke patients locally.
- Rapid decline, then stabilization—A sharp initial decrease shows the immediate impact of improved training and stroke protocols, followed by a steady, sustainable reduction.
- Hospitals became stroke-ready—Instead of immediately transferring patients, providers developed the expertise and confidence to assess, diagnose, and treat strokes on-site.
RBI’s impact is clear, hospitals don’t just recognize strokes better, they treat them better. By reducing transfers and strengthening local stroke care, more patients receive the right treatment at the right time, without having to leave their communities.
Provided Fast, Safe Treatment: Faster Action, Better Outcomes, Safer Care
Time is critical in stroke care. Before RBI’s intervention, hospitals often struggled with slow response times, delayed treatment, and higher complication rates. Many stroke teams took too long to activate, and door-to-needle times frequently exceeded the recommended treatment window.
RBI introduced standardized protocols, hands-on training, and streamlined activation processes, ensuring that stroke teams responded faster, treatment was administered sooner, and patient safety remained a top priority.
Key Takeaways from the Data:
- Faster Stroke Team Activation – Median door-to-stroke team time became three times faster than the national goal of under 15 minutes.
- Reduced Door-to-Needle Times – Treatment is now administered in under 30 minutes, ensuring more patients receive tPA within the critical window.
- Safer Stroke Treatment – RBI-trained hospitals maintain a 2.2% tPA hemorrhagic conversion rate, significantly lower than the 6% national average.
With RBI’s expertise, stroke teams don’t just work faster—they work smarter and safer. These improvements ensure that every second counts, every treatment is timely, and every patient has the best chance at recovery.
Achieved Extraordinary Patient Outcomes: Saving More Lives, Improving Recoveries
Stroke care isn’t just about survival, it’s about ensuring patients regain independence and quality of life. RBI’s approach has led to dramatic improvements in both survival rates and neurological recovery.
Key Takeaways from the Data:
- 37% reduction in stroke death rate for Native Americans—ensuring more patients survive and recover.
- 73% fewer neurological deficits (NIHSS score improvement) at discharge—meaning patients leave the hospital in far better condition.
- 52% of patients fully recovered—regaining normal neurological function.
- 84% of patients regained full independence—discharged with minimal to no long-term disability.
RBI’s impact is measurable, life-changing, and unmatched. By combining expert-led training, advanced stroke protocols, and a commitment to patient-centered care, we’re redefining what’s possible in stroke treatment and recovery.
Robust Outpatient Neuro Clinic Capacity: Expanding Access, Preventing Stroke
The ability to provide timely, high-quality outpatient neurology care is critical to preventing both initial and recurrent strokes. RBI has helped hospitals significantly expand their outpatient neuro capacity, ensuring more patients receive specialized neurological care faster than ever before.
Key Takeaways from the Data:
- Increased patient volume while maintaining high-quality care
- Cleared a 900-patient backlog 18 months ahead of schedule
- Established fellowship-trained subspecialty clinics, including MS, headache, and movement disorder clinics
This growth directly impacts stroke prevention—patients who receive timely neurological care are less likely to experience secondary strokes. With more patients seen sooner and highly trained specialists available, RBI is breaking the cycle of recurrent stroke and improving long-term neurological health.
Explore Case Studies
Services
Discover neurological care, from acute interventions to long-term support, tailored to meet every patient’s needs.
Team
Meet the experts redefining neurological care with passion, innovation, and collaboration to deliver exceptional care.
About
See how RBI transforms neurological care through innovation, expertise, and a commitment to better outcomes.